Identifying Vein Disease Symptoms:
The Key to Avoiding More Serious Health Conditions
Those unsightly and irritating varicose and spider veins aren’t just a cosmetic issue. If left untreated, they may lead to serious health complications such as deep vein thrombosis (DVT).
That’s why by learning more about the early signs of vein disease, you can save yourself from increased pain or complex treatments by seeking immediate expert evaluation and treatment from renowned board-certified vascular surgeon Dr. Joseph Magnant and his team of vein specialists at either one of our state-of-the-art offices in Fort Myers and Bonita Springs.
Understanding Vein Disease Symptoms and Signs
Just by visiting this web page, you are taking a valuable step. According to the Society for Vascular Medicine, more than 30 million Americans suffer from vein disease, but only 10% of people seek treatment for it. You are taking control of your health by learning more about your vein disease symptoms. The most common signs and symptoms of vein disease include:
You can see that what you may have thought were minor or cosmetic issues, are actually the tell-tale signs of something more serious.
What is the Difference Between Spider Veins and Varicose Veins?
This is one of the questions we get most often. The most common signs of vein disease include spider veins and varicose veins. Spider veins appear as smaller, more superficial veins. These look like a network of tiny red and purple spider web-like marks on the legs. Some people say they look like features on a map. Varicose veins are larger, swollen, blue and purple ropey veins easily visible upon a physical exam.
Varicose veins can cause discomfort in the form of heavy, swollen, tired, restless or achy legs. Sitting or standing in the same position such as during work can cause worsening symptoms throughout the day. Spider veins typically do not cause any symptoms, except for occasional minor discomfort in the form of a dull ache.


Early Evaluation of Vein Disease Ensures a Variety of Treatment Options
Everybody wants to believe that that their varicose veins or spider veins are like rashes – that they will eventually go away, but unfortunately, that’s not true. Left untreated, the vein disease that causes them generally progresses and they get worse. You can expect continued enlargement of the varicose veins and thinning of the overlying skin. If you have these vein disease symptoms now, they will almost assuredly get worse.
If they get really bad, it can lead to erosion of the skin and varicose vein bleeding or ulcers.
Physical appearance may not be the most important thing to consider about your current vein disease symptoms. Vein disease can also result in the development of Chronic Venous Insufficiency (CVI), which occurs when the valves in your leg veins fail to close tightly and allow blood to pool in your legs. Although usually not life threatening, CVI can result in significant medical complications.
How Serious Can Vein Disease Symptoms Get?
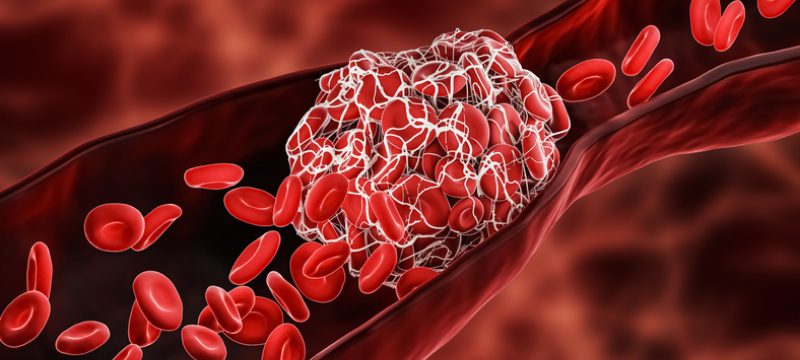
The most serious medical condition that can result from untreated vein disease, DVT, occurs when a blood clot forms in a varicose vein and extends to one or more of the deep veins inside your leg. This can lead to life-threatening pulmonary embolism (blood clots in the lungs) and must be treated promptly. That’s why it’s important you don’t stop at just reading this web page and schedule an early evaluation. This is critical in establishing the underlying cause of vein disease and expediting the most effective vein treatment options.


Get Leading Vein Disease Evaluation and Treatment from Vein Specialists
Designated as a Center for Excellence in Venous Care, Vein Specialists offers leading-edge vein treatment to get you the relief you deserve. We are the original IAC Accredited Vein Centers in Southwest Florida.
If you notice any of the vein disease symptoms listed above, schedule an evaluation with expert vein disease specialist Dr. Magnant at Vein Specialists today. You may also take our convenient online vein screening to see if you might be a candidate for a formal vein evaluation. We look forward to serving you!













