Today it is more important than ever for patients to take a more active role in researching their medical care. Fortunately, the internet has provided the means by which patients can perform background research on their health care providers’ training and experience and choose the most appropriate specialist.
Leg ulcers are a common source of distress for many patients and may have a variety of causes. The key to successful management of lower limb ulcers is determining the underlying problem as early in the treatment process as possible. Ulcers can be broadly classified into one of three etiologies: arterial, venous, or neuropathic.
 Arterial ulcers are typically characterized by extreme pain in a pale appearing wound which may have necrotic edges. Pulses may be absent or diminished, and the lower legs or feet may lack hair and the nails may be thickened. Patients may complain of pain in their feet across their toes when they elevate their legs in bed (rest pain). Risk factors for developing peripheral arterial disease (PAD), which is the underlying cause of arterial ulcers, are diabetes, advanced age, high blood pressure, cigarette smoking, high cholesterol and a strong family history. Incidental wounds or injuries often develop into non-healing ulcers in patients with PAD, examples of which include biopsy of a skin lesion, traumatic injury or a surgical incision. Often, these are insignificant wounds which would heal without delay in a patient with normal arterial circulation, but fester and grow in size in patients with compromised arterial supply. Accurate diagnosis can be established with non-invasive vascular laboratory testing and minimally invasive treatments are available which often involve the use of balloons, stents, LASERs and other devices which actually remove excess plaque and restore normal arterial blood flow. Delayed attention in a patient with an arterial ulcer may result in eventual amputation.
Arterial ulcers are typically characterized by extreme pain in a pale appearing wound which may have necrotic edges. Pulses may be absent or diminished, and the lower legs or feet may lack hair and the nails may be thickened. Patients may complain of pain in their feet across their toes when they elevate their legs in bed (rest pain). Risk factors for developing peripheral arterial disease (PAD), which is the underlying cause of arterial ulcers, are diabetes, advanced age, high blood pressure, cigarette smoking, high cholesterol and a strong family history. Incidental wounds or injuries often develop into non-healing ulcers in patients with PAD, examples of which include biopsy of a skin lesion, traumatic injury or a surgical incision. Often, these are insignificant wounds which would heal without delay in a patient with normal arterial circulation, but fester and grow in size in patients with compromised arterial supply. Accurate diagnosis can be established with non-invasive vascular laboratory testing and minimally invasive treatments are available which often involve the use of balloons, stents, LASERs and other devices which actually remove excess plaque and restore normal arterial blood flow. Delayed attention in a patient with an arterial ulcer may result in eventual amputation.
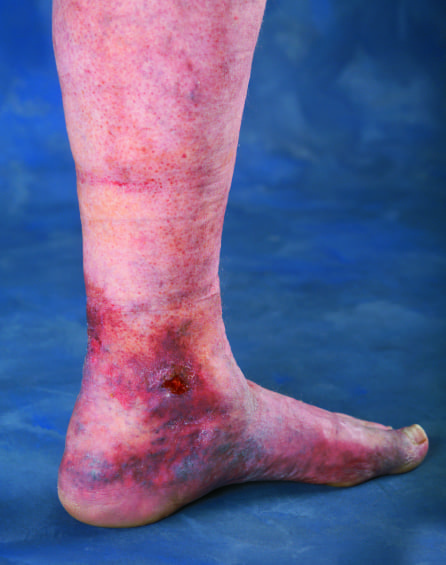
Venous ulcers are much more common than arterial ulcers and often affect a younger, healthier population. They typically appear in the area just above the ankle on the medial or inside surface of the calf, although they can occur in other areas as well. There is often a strong family history of venous insufficiency in patients with venous ulcers, and there may be other signs of venous insufficiency in these patients such as varicose veins, leg swelling or skin discoloration. Patients may also have a variety of vein disease symptoms including leg fatigue, achiness or pain which worsens by the end of the day, sitting, or standing and improves with elevation and walking. The underlying cause is venous hypertension, which if left untreated may lead to skin thickening and pigmentation (stasis dermatitis). Stasis dermatitis (or lipodermatosclerosis-fat and skin scarred to the underlying muscle tissue of the legs) is a precursor to ulceration, as minor injuries in diseased skin tend to heal poorly. Early investigation of the venous circulation by a qualified vein specialist, with a detailed venous insufficiency ultrasound will often disclose the culprit vein or veins with leaky valves. A variety of minimally invasive treatments are very effective and all share the same goal of sealing the leaking vein closed in an effort at returning the venous pressure to normal levels. Once this has been accomplished, ulcers often heal without much delay. In 15-20% of patients with venous ulcers, there may be a deeper, pelvic vein problem where the outflow veins are compressed or pinched. There are new methods of making this diagnosis and minimally invasive techniques for opening these blocked pelvic veins are very effective. If you have had a chronic lower extremity ulcer for more than 3 months and have not had a thorough vascular evaluation including the arterial and venous circulation, take the initiative to schedule an evaluation on your own.
Neuropathic ulcers are most common seen in diabetics as a result of deterioration of the peripheral nerves and subsequent weakening of the bonds which hold the bones of the feet together. Muscles often atrophy and the normal architecture of the feet change resulting in weight bearing on improper parts of the feet which leads to callus formation. Neuropathy my also result in a wound not being recognized, especially on the plantar surface of the feet, which may lead to serious infections of the deep soft tissue and bones in more severe cases. Pulses in diabetics may be normal or diminished based on the age of the patient and whether there is also a history of arterial disease. Diabetic neuropathy is usually not affected by the time of day and is often described as a stocking glove distribution.
Regardless of the etiology of a lower extremity wound, they should be taken seriously and treated with a sense of urgency, as the mere presence of an open wound serves as a portal of entry for bacteria to enter the blood stream and risk infecting existing artificial joints, heart valves and bone spurs of the spine and other bones. Rather than just treating the wound with a variety of topical agents, it is critical to identify the root cause of the ulcer and obtain trained professional care for the underlying problem. I have seen too many patients suffering for years with ulcers of indeterminate cause, only to be found to have straight forward venous disease. Once the underlying venous disease is identified and treated appropriately, the ulcers heal within 4-6 weeks with patient directed wound care. In conclusion, if you have a non-healing wound, you deserve a thorough assessment to determine the underlying cause.
Vein Specialists has offices in Fort Myers and Bonita Springs and is a leading outpatient vein center in Southwest Florida. Vein Specialists is committed to excellence in vein care and is dedicated to increasing physician and public awareness of venous disease. For more information about vein disease and Vein Specialists, please visit WeKnowVeins.com or call 239.694.8346.
Call Or Request An Appointment
Contact us to schedule an appointment with our expert Vein Specialists team. We will evaluate your signs and symptoms, answer your questions, and create a personalized vein care treatment plan to relieve your leg pain and enhance your life.
Schedule Your Appointment TodayRequest an Appointment
Please take a moment and fill out your request below and one of our staff members will be in contact within 24-48 business hours. If this is an emergency, call 911 immediately. If this is a non-emergent concern, please call the office Monday-Friday between 8am – 5pm at: 239-694-8346


